Understanding Type 1 Diabetes: A Comprehensive Guide
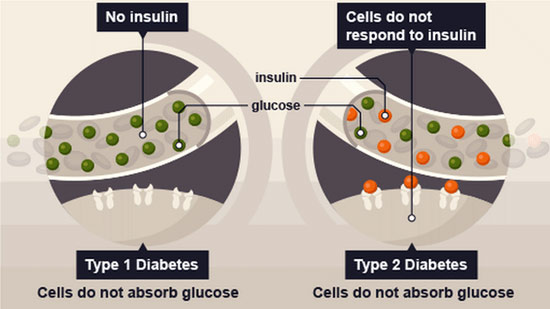
Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition characterized by the pancreas’s inability to produce sufficient insulin. Insulin is a hormone vital for regulating blood sugar levels and facilitating the uptake of glucose into cells for energy. Without enough insulin, glucose builds up in the bloodstream, leading to high blood sugar levels, which can result in various complications if left untreated.
What Causes Type 1 Diabetes?
Type 1 diabetes is an autoimmune disease, meaning the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. While the exact cause of this autoimmune response remains unclear, genetic predisposition and environmental factors likely play significant roles.
Genetic Factors
Research suggests that certain genes increase the risk of developing type 1 diabetes. Individuals with specific human leukocyte antigen (HLA) genotypes have a higher susceptibility to autoimmune reactions targeting pancreatic beta cells. However, not everyone with these genetic markers develops the condition, indicating that environmental triggers also contribute to disease onset.
Environmental Triggers
Various environmental factors may trigger the autoimmune response leading to type 1 diabetes. These triggers can include viral infections, such as enteroviruses, exposure to certain dietary components early in life, such as cow’s milk proteins, and other unidentified environmental factors. Additionally, factors like geography and seasonality may influence disease prevalence, suggesting a complex interplay between genetic susceptibility and environmental triggers.
Symptoms of Type 1 Diabetes
The symptoms of type 1 diabetes typically develop rapidly over a short period, often within weeks or even days. Recognizing these symptoms is crucial for prompt diagnosis and management of the condition. Common symptoms include:
- Excessive thirst: Increased thirst (polydipsia) is a hallmark symptom of high blood sugar levels. The body attempts to flush out excess glucose through urine, leading to frequent urination and dehydration.
- Frequent urination: Excess glucose in the bloodstream overwhelms the kidneys’ ability to reabsorb it, resulting in increased urine production (polyuria).
- Unexplained weight loss: Despite increased appetite and food intake, individuals with type 1 diabetes may experience unexplained weight loss due to the body’s inability to utilize glucose for energy.
- Fatigue: Insufficient glucose uptake by cells leads to energy depletion, causing persistent fatigue and weakness.
- Blurry vision: High blood sugar levels can cause fluid imbalances in the eye, leading to temporary changes in vision.
- Increased hunger: Cells deprived of glucose signal hunger, even when food intake is adequate.
Diagnosing Type 1 Diabetes
Diagnosing type 1 diabetes typically involves a combination of medical history, physical examination, and laboratory tests. Healthcare providers may perform the following diagnostic tests:
Blood Glucose Testing
Measuring blood glucose levels using a blood glucose meter provides immediate insights into an individual’s blood sugar levels. Fasting blood sugar tests and random blood sugar tests are commonly used to diagnose diabetes.
Glycated Hemoglobin (A1C) Test
The A1C test measures average blood sugar levels over the past two to three months by assessing the percentage of hemoglobin molecules bound to glucose. Elevated A1C levels indicate poor blood sugar control and may suggest diabetes.
C-peptide Test
The C-peptide test measures the level of C-peptide, a byproduct of insulin production, in the blood. Low levels of C-peptide coupled with low insulin levels indicate type 1 diabetes, as the pancreas fails to produce sufficient insulin.
Managing Type 1 Diabetes
Managing type 1 diabetes requires a comprehensive approach aimed at controlling blood sugar levels, preventing complications, and maintaining overall health. Treatment strategies typically include:
Insulin Therapy
Since individuals with type 1 diabetes cannot produce insulin, insulin therapy is essential for managing blood sugar levels. Various insulin formulations, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin, may be prescribed based on individual needs.
Blood Sugar Monitoring
Regular monitoring of blood sugar levels using a blood glucose meter helps individuals with type 1 diabetes adjust their insulin doses, diet, and physical activity levels to maintain optimal blood sugar control.
Healthy Eating
Following a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is essential for managing blood sugar levels and preventing complications associated with type 1 diabetes.
Regular Exercise
Engaging in regular physical activity helps improve insulin sensitivity, lower blood sugar levels, and enhance overall health. Activities like brisk walking, cycling, swimming, and strength training are beneficial for individuals with type 1 diabetes.
Continuous Glucose Monitoring (CGM)
CGM systems provide real-time insights into blood sugar levels, allowing for more precise diabetes management and reducing the risk of hypoglycemia and hyperglycemia.
Complications of Type 1 Diabetes
Untreated or poorly managed type 1 diabetes can lead to various short-term and long-term complications affecting multiple organ systems. Common complications include:
- Hypoglycemia: Low blood sugar levels can cause symptoms like shakiness, confusion, dizziness, and, if severe, loss of consciousness.
- Hyperglycemia: Prolonged high blood sugar levels can lead to diabetic ketoacidosis (DKA), a life-threatening condition characterized by ketone buildup in the blood.
- Cardiovascular Disease: Diabetes increases the risk of developing cardiovascular diseases such as heart attack, stroke, and peripheral artery disease.
- Nephropathy: Diabetes-related kidney damage (diabetic nephropathy) can lead to chronic kidney disease and eventual kidney failure.
- Neuropathy: Nerve damage caused by diabetes (diabetic neuropathy) can result in symptoms like numbness, tingling, pain, and loss of sensation in the extremities.
Conclusion
Type 1 diabetes is a complex chronic condition that requires lifelong management to maintain optimal health and prevent complications. By understanding the underlying causes, recognizing symptoms, obtaining timely diagnosis, and implementing appropriate treatment strategies, individuals with type 1 diabetes can lead fulfilling lives while effectively managing their condition.